When considering birth control options, the intrauterine device (IUD) often emerges as a popular choice due to its long-lasting and effective nature. However, like any medical intervention, it is crucial to be informed about the potential side effects associated with its use. Understanding these side effects can help individuals make an informed decision that aligns with their health needs and lifestyle preferences.
With a variety of IUDs available in the market, each type comes with its own set of characteristics and potential side effects. Whether you're considering a hormonal IUD or a copper IUD, it's important to weigh the benefits against the possible drawbacks. Some people experience minimal side effects, while others might face more significant challenges. This article aims to provide a comprehensive look at the side effects you might encounter, equipping you with the knowledge to have an informed discussion with your healthcare provider.
In addition to exploring the side effects, we will also delve into frequently asked questions, providing clarity on common concerns. From understanding the differences between types of IUDs to knowing what to expect during the insertion process, this guide is designed to support your journey in choosing the right birth control method. By shedding light on the potential side effects and addressing key questions, this article aims to empower you with the information necessary to make a choice that's right for you.
Read also:Sandra Bullock Age Biography And More
Table of Contents
- What is an IUD?
- Types of IUDs
- How Do IUDs Work?
- Common Side Effects of IUDs
- What Are the Possible Long-Term Side Effects?
- Can IUDs Cause Hormonal Imbalances?
- Managing Pain and Discomfort
- Impact on Menstrual Cycle
- How to Handle Irregular Bleeding?
- IUD Expulsion and Other Complications
- What Should You Know About Insertion and Removal?
- Infection Risks Associated with IUDs
- IUDs and Fertility Concerns
- Frequently Asked Questions
- Conclusion
What is an IUD?
An intrauterine device (IUD) is a small, T-shaped device inserted into the uterus to prevent pregnancy. It's a form of long-acting reversible contraception (LARC), which means it provides long-term birth control but can be removed at any time if a woman decides to become pregnant. The device is highly effective, with a success rate of over 99%, making it a popular choice among those seeking reliable contraception.
IUDs come in two main types: hormonal and copper. Both types are inserted by a healthcare professional during a brief office procedure. The choice between a hormonal or copper IUD often depends on personal preferences, health considerations, and how the body might react to the device. Each type has its own mechanism of action and potential side effects, which we'll explore in further detail.
Understanding what an IUD is and how it functions is crucial for making an informed decision. It's important to consult with a healthcare provider to discuss any health conditions or concerns that might affect the suitability of an IUD for your contraceptive needs. With the right information, you can choose the option that best fits your lifestyle and reproductive goals.
Types of IUDs
There are two main categories of IUDs: hormonal and copper. Each type has distinct features and potential side effects, which can influence your choice based on personal health needs and preferences.
Hormonal IUDs
Hormonal IUDs release small amounts of progestin, a hormone similar to progesterone, into the uterus. This hormone works by thickening the cervical mucus to block sperm and, in some cases, by thinning the uterine lining to prevent implantation. Hormonal IUDs include brands such as Mirena, Kyleena, Liletta, and Skyla. They generally last between 3 to 7 years, depending on the type.
Copper IUDs
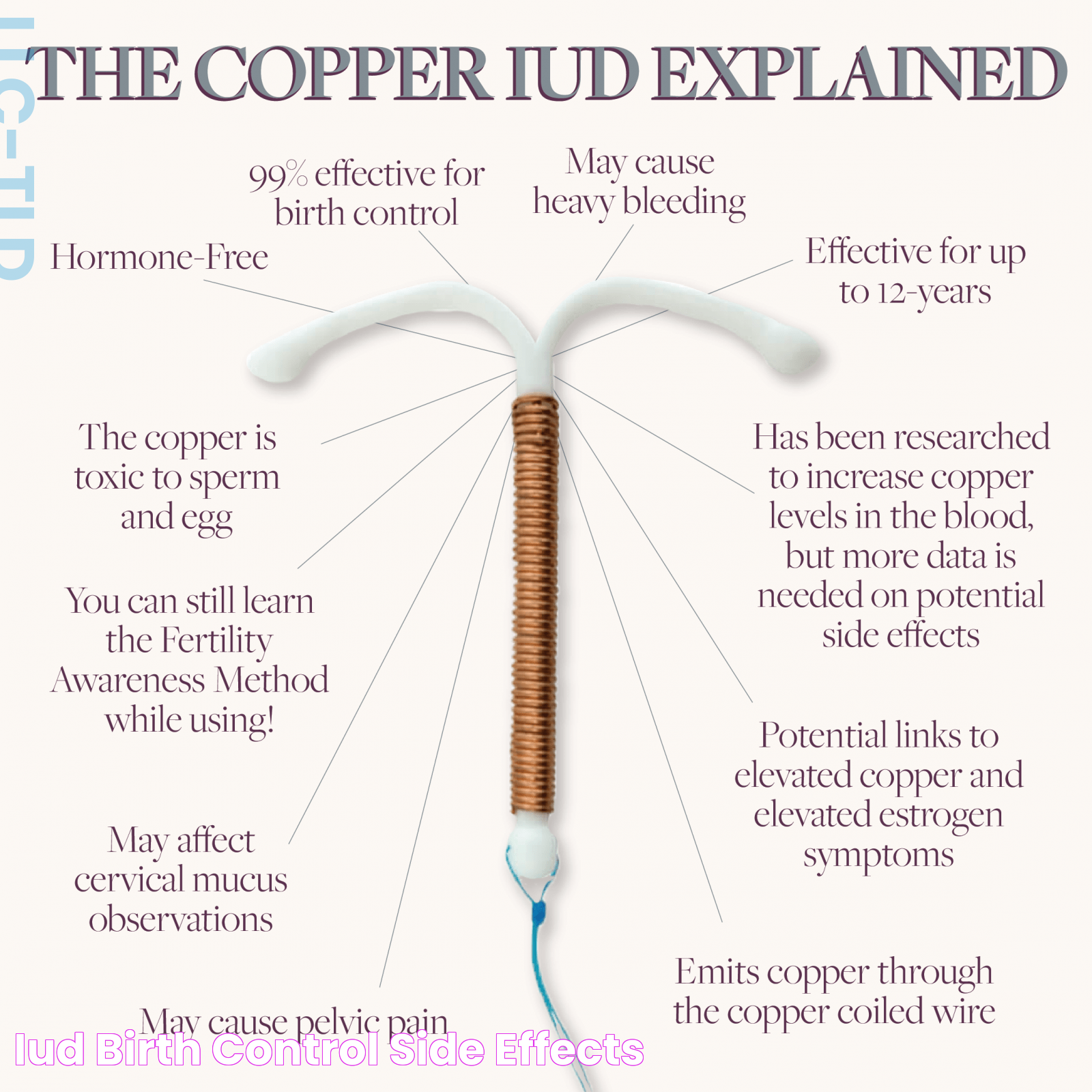
Copper IUDs, such as ParaGard, do not contain hormones. Instead, they use copper wire coiled around the device to create an environment that's toxic to sperm. The presence of copper triggers an inflammatory response in the uterus, which prevents sperm from fertilizing an egg. Copper IUDs can last up to 10 years, making them a long-term, hormone-free contraceptive option.
Read also:Deciphering The Sigma Male Definition An Indepth Analysis
Both types of IUDs are effective in preventing pregnancy, but their differences in composition and mechanism can lead to varying side effects. It's important to discuss these differences with a healthcare provider to determine which IUD might be the best fit for your body and lifestyle.
How Do IUDs Work?
IUDs are designed to prevent pregnancy through different mechanisms, depending on whether they are hormonal or copper-based. Understanding these mechanisms can help you make an informed choice about which type of IUD might be right for you.
Hormonal IUD Mechanism
The hormonal IUD releases levonorgestrel, a synthetic form of the hormone progesterone, directly into the uterus. This hormone thickens the cervical mucus, making it difficult for sperm to enter the uterus and reach an egg. Additionally, it can thin the lining of the uterus, reducing the likelihood of implantation. In some cases, hormonal IUDs may also suppress ovulation, further decreasing the chance of pregnancy.
Copper IUD Mechanism
The copper IUD works by releasing copper ions into the uterus, creating an inflammatory reaction that is toxic to sperm. This hostile environment prevents sperm from fertilizing an egg. Unlike hormonal IUDs, copper IUDs do not alter a woman's hormonal balance, making them a suitable option for those who prefer a non-hormonal contraceptive method.
Both types of IUDs offer effective protection against pregnancy, but their mechanisms of action can lead to different side effects and considerations. It's important to understand how each type works to determine which IUD aligns with your health and lifestyle goals.
Common Side Effects of IUDs
While IUDs are generally safe and effective, they can cause side effects in some individuals. Being aware of these potential side effects can help you prepare and manage them if they occur.
Pain and Cramping
Many women experience pain and cramping during and after IUD insertion. This discomfort is usually temporary and can be managed with over-the-counter pain medications like ibuprofen. Some individuals may also experience cramping during their menstrual periods, especially in the first few months after insertion.
Spotting and Irregular Bleeding
Spotting and irregular bleeding are common side effects, particularly with hormonal IUDs. These irregularities often decrease over time as the body adjusts to the device. For some women, periods may become lighter or stop altogether with hormonal IUDs. Copper IUDs, on the other hand, may initially cause heavier periods and more intense cramping, although these symptoms often lessen over time.
Hormonal Side Effects
For those using hormonal IUDs, there may be additional side effects related to the hormone release, such as acne, breast tenderness, headaches, and mood changes. These side effects are generally mild and tend to improve after a few months of use.
Understanding these common side effects and how to manage them can help you navigate the initial adjustment period after getting an IUD. It's important to keep in touch with your healthcare provider if side effects persist or become severe.
What Are the Possible Long-Term Side Effects?
While many side effects of IUDs are temporary, some individuals may experience long-term effects. It's important to be aware of these potential outcomes when considering an IUD for contraception.
Impact on Menstrual Cycle
For hormonal IUD users, long-term changes to the menstrual cycle can occur. Some women experience lighter periods or may stop menstruating altogether. While this is not harmful, it can be a significant change that some individuals may need to adjust to. Copper IUDs, on the other hand, may result in longer or heavier periods, although these changes often stabilize after the first few months.
Pelvic Inflammatory Disease (PID)
There is a slight increased risk of developing pelvic inflammatory disease (PID) shortly after IUD insertion, particularly if there is a pre-existing sexually transmitted infection (STI) at the time of insertion. However, the overall risk remains low when proper screening and precautions are taken.
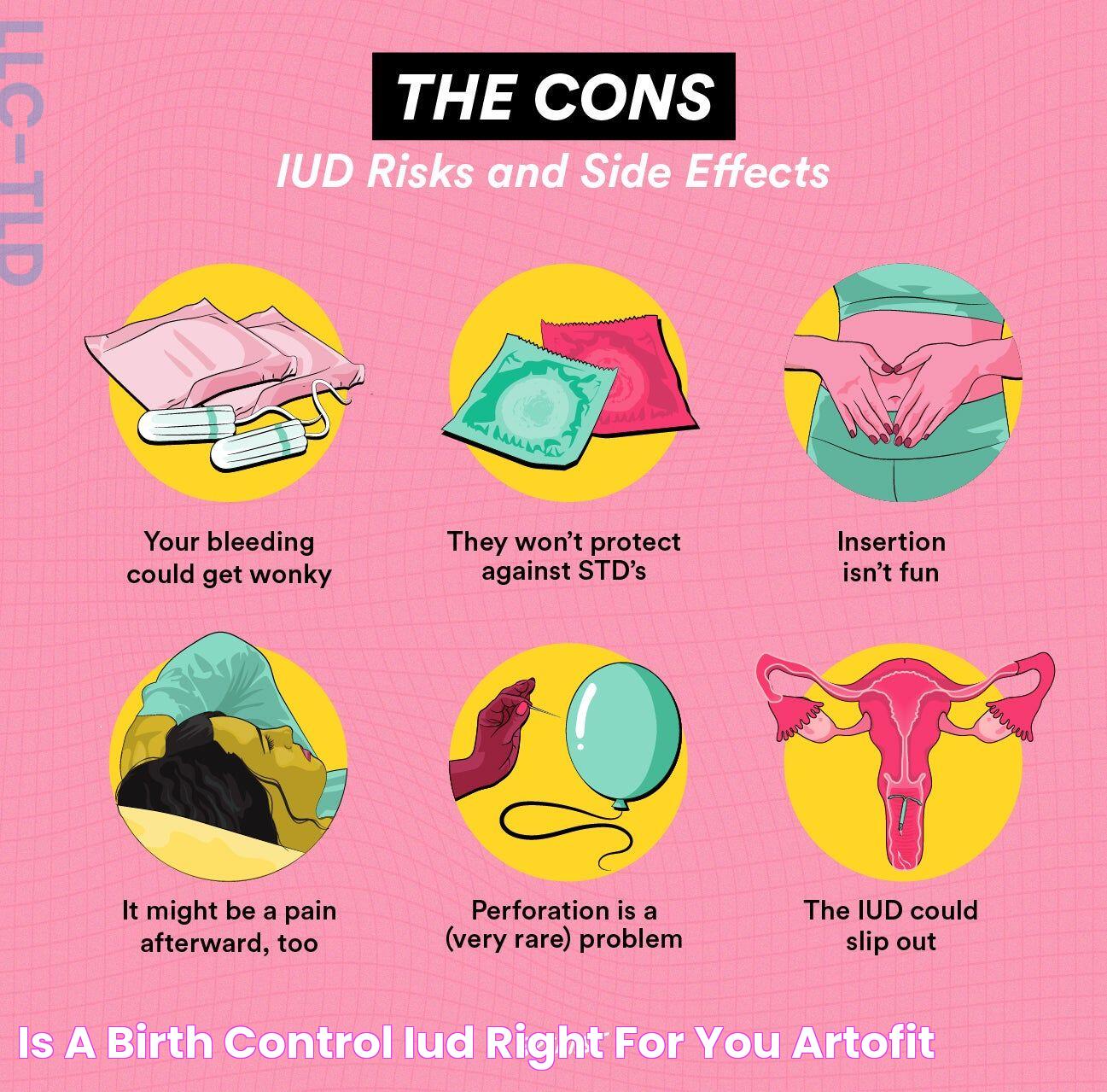
Perforation and Expulsion
In rare cases, an IUD may perforate the uterine wall or become expelled from the uterus. These complications can lead to discomfort and may require medical intervention. Regular check-ups with a healthcare provider can help ensure the IUD is in the correct position.
Being informed about these potential long-term side effects allows you to weigh the benefits and risks of using an IUD as your chosen method of contraception. Regular consultations with a healthcare provider can help manage any concerns that arise.
Can IUDs Cause Hormonal Imbalances?
One common concern regarding hormonal IUDs is their potential to cause hormonal imbalances. Understanding how these devices interact with your body's natural hormone levels can help address these concerns.
Hormonal Influence
Hormonal IUDs release a small, localized amount of progestin, which primarily affects the uterus. Unlike other hormonal contraceptives, such as birth control pills or patches, the systemic absorption of hormones from an IUD is minimal. This localized action means that hormonal IUDs are less likely to cause widespread hormonal imbalances.
Side Effects Related to Hormonal Changes
Some users may experience side effects such as mood swings, acne, or breast tenderness, which can be attributed to hormonal changes. These side effects are usually mild and tend to improve over time as the body adjusts to the device.
While hormonal IUDs can influence your hormone levels, they are generally considered safe and effective for most individuals. If you have concerns about hormonal imbalances, it's important to discuss them with your healthcare provider, who can offer guidance and reassurance based on your individual health profile.
Managing Pain and Discomfort
Pain and discomfort are common concerns for those considering an IUD. However, there are several strategies to manage these symptoms effectively.
Before and During Insertion
- Discuss pain relief options with your healthcare provider before the procedure.
- Consider taking an over-the-counter pain reliever, such as ibuprofen, an hour before insertion.
- Practice deep breathing techniques or meditation to help relax during the procedure.
Post-Insertion Care
- Continue taking pain relievers as needed for cramping and discomfort.
- Apply a heating pad to the lower abdomen to ease cramping.
- Rest and avoid strenuous activities for a day or two after insertion.
By preparing for the insertion process and knowing how to manage post-insertion discomfort, you can make the experience more manageable. It's important to communicate with your healthcare provider if you experience severe pain or if discomfort persists.
Impact on Menstrual Cycle
IUDs can have a significant impact on your menstrual cycle, depending on the type used. Understanding these changes can help you adjust and plan accordingly.
Hormonal IUDs
Many users of hormonal IUDs experience lighter periods, and some may stop menstruating altogether. This change occurs due to the thinning of the uterine lining, which reduces menstrual bleeding. While the absence of periods can be concerning for some, it's a normal side effect and not indicative of any health issues.
Copper IUDs
Copper IUDs may initially cause heavier periods and more intense cramping, particularly in the first few months after insertion. These symptoms typically decrease over time as the body adjusts to the device. If heavy bleeding persists, it's important to consult with a healthcare provider to rule out any underlying issues.
Being aware of how an IUD might affect your menstrual cycle can help you prepare for these changes and manage any concerns that arise. It's important to maintain open communication with your healthcare provider to address any persistent or severe symptoms.
How to Handle Irregular Bleeding?
Irregular bleeding is a common side effect for IUD users, particularly in the first few months after insertion. Here are some strategies for managing this symptom:
Monitor Your Cycle
- Keep track of your bleeding patterns using a calendar or mobile app.
- Note any changes in flow, duration, or frequency of bleeding.
Communicate with Your Healthcare Provider
- Discuss any concerns or significant changes in bleeding patterns.
- Seek medical advice if bleeding is excessively heavy or prolonged.
By monitoring your cycle and maintaining open communication with your healthcare provider, you can effectively manage irregular bleeding and address any concerns that arise.
IUD Expulsion and Other Complications
While IUDs are generally safe and effective, there are some potential complications to be aware of, including expulsion and perforation.
IUD Expulsion
Expulsion occurs when the IUD partially or completely comes out of the uterus. This can happen if the IUD is not properly positioned or if the uterus contracts strongly during menstruation. Signs of expulsion include feeling the IUD in the cervix or experiencing unusual pain or bleeding. If you suspect expulsion, it's important to contact your healthcare provider for evaluation and potential reinsertion.
Uterine Perforation
Perforation is a rare complication in which the IUD punctures the uterine wall. This can occur during insertion or if the IUD moves out of place. Symptoms of perforation include severe pain, heavy bleeding, or signs of infection. If perforation is suspected, medical intervention is necessary to remove the IUD and assess any damage.
Being aware of these potential complications and knowing the signs to watch for can help you seek timely medical intervention if needed. Regular check-ups with your healthcare provider can also help ensure the IUD remains in the correct position.
What Should You Know About Insertion and Removal?
Understanding the insertion and removal process for an IUD can help you prepare for these procedures and know what to expect.
Insertion Process
IUD insertion is a quick outpatient procedure performed by a healthcare provider. During the procedure, the provider will use a speculum to visualize the cervix and insert the IUD through the cervical canal and into the uterus. The process usually takes only a few minutes, and most individuals experience some cramping and discomfort during and after the procedure.
Removal Process
IUD removal is also a straightforward procedure. The healthcare provider will use a speculum to access the cervix and then gently pull on the IUD strings to remove the device. Most individuals experience mild discomfort during removal, but the process is typically quick and uncomplicated.
Being informed about the insertion and removal processes can help alleviate anxiety and ensure you are prepared for these procedures. It's important to follow any pre- and post-procedure instructions provided by your healthcare provider to ensure a smooth experience.
Infection Risks Associated with IUDs
While IUDs are generally safe, there is a small risk of infection associated with their use, particularly shortly after insertion.
Risk Factors
The risk of infection is highest in the first three weeks following IUD insertion. This risk is primarily related to the introduction of bacteria into the uterus during the insertion process. The presence of a pre-existing sexually transmitted infection (STI) can also increase the risk of developing pelvic inflammatory disease (PID) after IUD insertion.
Preventive Measures
- Undergo STI screening before IUD insertion to reduce the risk of PID.
- Follow your healthcare provider's instructions for post-insertion care to minimize infection risk.
- Monitor for signs of infection, such as fever, unusual discharge, or severe pelvic pain, and seek medical attention if these symptoms occur.
By being aware of the infection risks and taking appropriate preventive measures, you can reduce the likelihood of complications and ensure the safe use of an IUD.
IUDs and Fertility Concerns
Many individuals considering an IUD may have questions about how the device might affect their fertility in the future. Understanding the relationship between IUDs and fertility can provide reassurance.
Reversible Contraception
IUDs are a form of long-acting reversible contraception (LARC), meaning that they do not have a lasting impact on fertility. Once the IUD is removed, fertility generally returns to normal, allowing individuals to conceive if they choose to do so.
Time to Conception
Most individuals can conceive soon after IUD removal, with no significant delay in fertility. However, factors such as age, overall health, and underlying fertility issues can influence the time it takes to become pregnant after IUD removal.
Understanding that IUDs do not have a lasting impact on fertility can provide peace of mind for those considering this form of contraception. If you have specific concerns about fertility, it's important to discuss them with your healthcare provider.
Frequently Asked Questions
Do IUDs cause weight gain?
There is no strong evidence to suggest that IUDs cause significant weight gain. Some individuals may experience mild changes in weight due to hormonal fluctuations, but these changes are typically minimal.
Can I use an IUD if I've never been pregnant?
Yes, IUDs are suitable for individuals who have never been pregnant. Healthcare providers can determine the appropriate IUD size and type based on your individual anatomy and health needs.
How soon can I have sex after IUD insertion?
It's generally recommended to wait 24 to 48 hours after IUD insertion before engaging in sexual activity. This allows time for the body to adjust and reduces the risk of expulsion.
What should I do if I can't feel the IUD strings?
If you cannot feel the IUD strings, it's important to contact your healthcare provider for an examination to ensure the IUD is in the correct position. Do not attempt to locate the strings yourself, as this can cause displacement.
Can an IUD be used as emergency contraception?
A copper IUD can be used as emergency contraception if inserted within five days of unprotected intercourse. It is highly effective as an emergency contraceptive method.
How often should I check my IUD strings?
It's advisable to check your IUD strings monthly, usually after your period, to ensure the device remains in place. If you notice any changes, contact your healthcare provider for further evaluation.
Conclusion
Intrauterine devices (IUDs) offer a highly effective and long-lasting form of contraception, but like any medical intervention, they come with potential side effects and considerations. Understanding these side effects, from common symptoms like cramping and irregular bleeding to rare complications such as expulsion and perforation, is crucial for making an informed decision about using an IUD.
By being well-informed about the different types of IUDs, their mechanisms, and how they might affect your body, you can have a productive conversation with your healthcare provider and choose the best contraceptive method for your needs. Regular check-ups and open communication with your healthcare provider are key to ensuring the safe and effective use of an IUD.
Ultimately, the decision to use an IUD should be based on a thorough understanding of the potential side effects, personal health considerations, and lifestyle preferences. With the right information and support, you can make a choice that aligns with your reproductive goals and enhances your overall well-being.